
The groundbreaking technology in the Pears Maudsley Centre

At the Pears Maudsley Centre, clinicians and researchers will collaborate with young people to improve the research and treatment of mental health and neurodevelopmental disorders.
At the heart of this centre will be the Clinical Research Facility (CRF), which is set to be the leading facility in the UK dedicated to the investigation and treatment of mental health in children and young people. The CRF will be a space where children of all ages, from babies upwards, can participate in research to identify the root of mental health and neurodevelopmental disorders, and use this research to implement and monitor groundbreaking interventions.
Supported by £11m of funding from the UK Research Partnership Investment Fund (UKRPIF) to King’s College London, the CRF will house cutting-edge technology to support pioneering mental health research with a particular focus on brain imaging. The equipment selected is aimed to be the least restrictive and intrusive, creating better experience for patients and participants. Much of this technology can be used together simultaneously to provide a more fully-formed, inclusive investigation and collaborative understanding of research.
Below is a comprehensive list of the technology which will be used at the CRF, detailing its application and how it will support research and interventions for aiding the mental health of children and young people.
Electroencephalography (EEG) Suite:
EEG is a non-invasive method that measures electrical activity in the brain through electrodes placed on the scalp. The CRF will have a specially shielded room for EEG which minimises electromagnetic interference from external sources such as electronic devices, which can distort these brain activity signals being measured.
Use in research: EEG is used to study brain activity patterns associated with various mental health and neurodevelopmental conditions such as autism, ADHD, depression and anxiety, thereby helping to advance our understanding of brain function and neurological disorders.

Credit: Cerca Magnetics
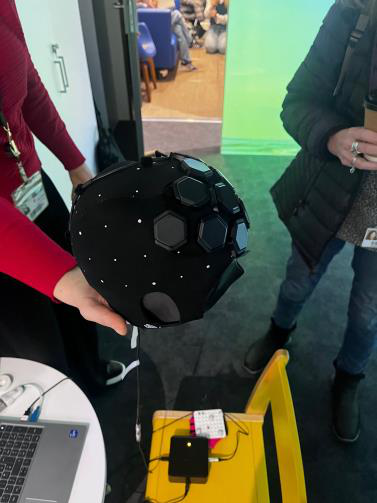
Optically Primed Magnetoencephalography (OPM-MEG) Scanner
The OPM-MEG is a new way to non-invasively assess brain function. It measures magnetic fields produced by brain activity with high temporal and spatial resolution. This means it can precisely record rapid changes in brain activity (such as individual neural events or quick changes in cognition) as well as accurately identify the specific brain regions where the changes happen. Unlike conventional MEG, this system can adapt to any age group (baby to adult) and patients can move freely during scanning.
Use in research: OPM-MEG provides insights into brain activity and underlying cognitive processes, improving understanding of neural mechanisms to aid the development of targeted interventions for conditions such as epilepsy, autism, ADHD.

Credit: Magstim
Virtual Reality (VR) Suite: Virtual Reality Cave + Virtual Reality Lab
The VR CAVE is a unique virtual reality laboratory featuring an immersive audio-visual environment that simulates real-world settings. It utilizes four-sided projection onto three walls and the floor, employing specialized technology and programming to create a 3D immersive experience. This can be used to simulate an environment for children and young people to help monitor their reactions and brain activity in response to stimulus in the simulated environment.
The Virtual Reality Lab will use cutting edge VR headsets, web-based platforms and “extended reality” (augmented reality, virtual reality, and mixed reality) which allows researchers to safely immerse participants in purpose-made scenarios, provoking similar cognitive, behavioural, and physical responses to real life within a controlled environment.
Use in research: Virtual reality, combined with motion tracking cameras, custom wearables and head-mounted eye tracking, provides an integrated platform that allows researchers to monitor, track and record brain activity and behaviour changes in conditions such as autism, depending on the simulated world around them.

Credit: Mechdyne
Functional near-infrared spectroscopy (fNIRS)
fNIRS is a non-invasive neuroimaging technique used to measure brain activity by monitoring local changes in blood oxygenation and blood volume in the brain. These changes indicate neural activity because they reflect local changes in blood flow and oxygen metabolism that occur in response to neuronal activation and brain excitation.
Use in research: fNIRS is used to investigate brain function and connectivity in mental health disorders, and to explore potential therapeutic interventions. fNIRS is well-suited for studying brain function in natural settings as it can withstand moving around, such as during social interactions or while participants are performing motor tasks. It is relatively easy to set-up and use and good for participants such as infants, children, and individuals with movement disorders who may move about a lot and have difficulty with other imaging methods such as MRI or EEG.
fNIRS (Lumo) cap at the Toddlerlab, Birkbeck University
Brain Stimulation
The use of brain stimulation techniques aims to investigate alternatives or adjuncts to traditional treatments like medication and psychotherapy for children & young people. These include:
- Transcranial Magnetic Stimulation (TMS)
- Transcranial direct current stimulation (tDCS)
- Transcranial Alternating Current Stimulation (tACS)
- Transcranial Random Noise Stimulation (tRNS)
These use electrodes to create magnetic fields or low electrical currents in different forms and frequencies in order to stimulate nerve cells or modulate and impacting brain activity.
Use in research: By directly influencing brain activity, these various brain stimulation techniques aim to correct neural dysfunctions underlying various mental health conditions. Research in this area will better understand their mechanisms of the developing brain, optimise brain stimulation applications, and expand their therapeutic uses.
Eye-tracking Suite
Eye trackers are another non-invasive method to explore underlying mechanisms of the brain and mental disorders. They monitor eye movements and gaze patterns to understand visual stimuli, attention and cognitive processes.
Use in research: Eye-tracking is used to study attentional biases, social cognition deficits, and emotional processing in disorders such as autism, depression, and anxiety.
Credit: Tobii
Data Capture Suite (including 3D printer)
The Data Capture Suite will use state-of-the art computing equipment, software and e-Health to build purpose-built digital tools, apps and investigate health data (including patient records).
Use in research: The data capture room infrastructure will be able to manage, analyse, and interpret large and complex datasets, leading to a deeper understanding of mental health and neurodevelopmental disorders that will enable clinicians and researchers to work towards effective interventions and treatments. It will allow information and data to play a vital role in clinical priorities such as prevention, reducing digital harms, health monitoring and targeted interventions.
Mobile Magnetic Resonance Imaging (MRI) and Functional MRI (fMRI)
The Mobile MRI is a portable brain imaging system that combines an ultra- low-field magnetic resonance with artificial intelligence. Unlike conventional MRI systems, it does not require extensive shielding and is small enough to be portable, which allows researchers to conduct brain-imaging studies in alternate settings (such as in clinical rooms or bedside), thus making them more accessible.
The high-powered functional MRI (fMRI) machine measures changes in blood flow in order to detect brain activity associated with cognitive processes, emotions, and mental health disorders.
Use in research: These imaging techniques help identify structural and functional abnormalities in mental health disorders and evaluate the effects of interventions on brain activity.

Credit: Hyperfine
Sound Research Lab
The Sound Research Lab refers to up to three specially equipped clinical consultation rooms installed with dedicated sound recording equipment and one that will be acoustically treated with sound insulation. This allows researchers to capture interviews and speech recordings to be analysed using specialist software and artificial intelligence.
Use in research: Sound research contributes to understanding auditory processing in different conditions and potentially provides indicators and biomarkers for clinicians via voice recognition.
Categories
Follow Us
For the latest updates and news, follow us on our social channels.










Recent Comments